Dr Saheb Sahu, FAAP, MPH
Introduction
Sickle cell disease (SCD) is an inherited blood disorder, passed down when both the parents carry the sickle cell gene. In such cases, there is a 25% chance that a child will inherit the disease.
The oldest known evidence of sickle cell disease has been traced back to more than 7,000 years. Researchers at National Institute of Health (NIH-USA) estimate that the sickle cell gene mutation (mutation is a change in the DNA sequence of an organism’s genome) first arose in the Sahara approximately 7,300 years ago and subsequently carried through African continent and outside by migration. At the time the mutation appeared, the Sahara was not a desert; it was green and wet and full of malaria causing mosquitoes. A type of malaria parasite has been identified in a fossil that dates back to 2 million years. The disease of malaria has been infecting humanity from our first emergence. A single copy of the gene effectively, having a sickle cell trait, conferred protection against severe malaria. Hence a muted gene which started as a protection against malaria, later on became the cause of sickle cell disease, when people migrated out of Africa.
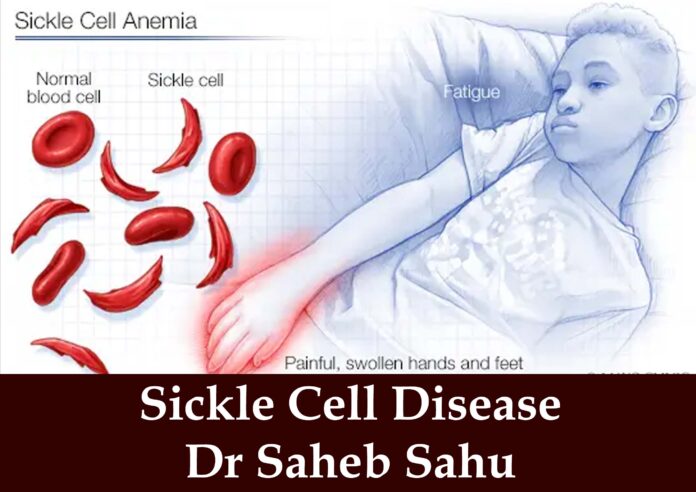
The illness was first described in medical literature more than a century ago. It was the first molecular disease to be understood, a single mutation in a single gene that causes a heritable illness. When someone has one copy of the gene, that person is often asymptomatic. But when someone inherits a copy from each parent, the disease can be excruciating. The mutation results in an abnormal hemoglobin, which causes the red blood cells to curve into a characteristic sickle shape and becomes stiff and sticky. Ultimately the sickled red blood cells fail to deliver oxygen efficiently to the tissues throughout the body. Untreated the disease can cause sepsis (blood infection), pneumonia, stroke, heart attack and punishing pain during a vaso-occlusive episodes or crises.
The disease affects as many as 20 million people around the world. Countries with the largest number of people with sickle cell disease are in Nigeria, The Republic of Congo and India. In the low-income countries where sickle cell disease is most prevalent and newborn screening for the disease is limited or nonexistent, too many children with sickle cell disease do not live past five years of age.
Prevalence of SCD in India
SCD has a significant presence in India, particularly among its tribal and scheduled casts population. SCD is more commonly found in the states of Maharashtra, Gujrat, Madhya Pradesh, Chhatisgarh, Odisha, Jharkhand, and parts of Andhra Pradesh and Telangana. The prevalence of sickle cell trait can range from 10% to 30% in different SC and ST population.
Signs and Symptoms of Sickle Cell Disease
The signs and symptoms of sickle cell disease (SCD) can vary widely and may range from mild to severe. They often begin to appear in infancy, typically around 5 months of age. Key signs and symptoms include:
1–Anemia: Since sickle cells break down prematurely, it leads to shortage of red blood cells, causing chronic anemia (low hemoglobin). This leads to symptoms such as fatigue, paleness, and shortness of breath.
2-Episodes of Pain (Pain crisis): These episodes occur when sickled red blood cells block blood flow through small blood vessels to the chest, abdomen, and joints. The pain can vary in intensity and duration, sometimes requiring hospitalization.
3- Swelling of Hands and Feet: Known as dactylitis, swelling of the hands and feet is often one of the first symptoms seen in infants with SCD.
4- Frequent Infections: Sickled cells can damage the spleen, an organ that helps fight infection, making individual with SCD more susceptible to infections early in life.
5- Delayed Growth and Puberty: Due to shortage of healthy red blood cells, children with SCD may experience slower growth and delayed puberty.
6- Acute Chest Syndrome: This is a severe condition similar to pneumonia, characterized by chest pain, fever, and difficulty in breathing. It can be life threatening.
Diagnosis of Sickle Cell Disease
The diagnosis of SCD is typically confirmed through blood tests that identify the presence of abnormal hemoglobin known as hemoglobin S (HbS). Here are the primary methods used for diagnosis:
1- Newborn Screening: In many countries, newborns are routinely screened for SCD shortly after birth, just by a heel stick. Early diagnosis leads to early intervention and better outcome.
2-Hemoglobin Electrophoresis: It is the most confirmatory test for SC D. This test can distinguish between having sickle cell trait, different forms of SCD, such as HbSS, HbSC, or HbS beta thalassemia.
3-Complete Blood Count (CBC) and Blood Smear: A CBC and blood smear can diagnose the severity of anemia and look into the sickle cell shape of the red blood cells.
4- Prenatal Testing: A pregnant woman can opt for prenatal testing to determine if the fetus she is carrying has SCD. This test is especially relevant for couples at risk of passing the disease to their children (e.g. when both parents are carrier of sickle cell trait).
New Therapies
Chemist Linus Pauling, later on a two-time winner of Nobel Prize, identified the hemoglobin of SCD as mutant molecule in 1949. Pauling dubbed sickle cell anemia as a “molecular disease”. That framing effectively launched the biomedical era of newly powerful laboratory research.
One of the first drugs to meaningfully help patients was penicillin, which was available in US in 1945. Sickling makes children more vulnerable to a variety of infections. Antibiotics made it possible to cure those infections. Twice daily doses of antibiotics are still routinely prescribed for children younger than five years who have sickle cell disease.
The first drug that made an impact on the disease process of sickle cell was a compound called hydroxyurea. It was originally a cancer drug, but it was approved for sickle cell disease by US Food and Drug Administration (FDA)until the 1990s.
In 1997 researchers established that periodic blood transfusions could reduce the risk of stroke in children diagnosed with sickle cell disease.
In 2007, researchers in France demonstrated that children with sickle cell could be cured with a bone marrow transplant from a donor who was an exact immunological match, such as a full sibling.
A burst of innovations in the past decade brought three new drugs into sickle cell care: L-glutamine approved in 2017, and Crizanlizumab and Voxelotor, both approved in 2019. The drugs are expensive and their uses have been slow.
The new gene therapies are extraordinary scientific achievement, but they are very expensive and difficult to obtain. Two patients in USA have recently been cured of the disease by gene therapy with an average cost of 3 million dollars each.
Prevention
Prevention of SCD focuses mainly on genetic counseling and screening of the newborns in the high-risk communities.
1-Genetic counselling: Individuals, especially those with family history of the disease or who belong to communities with higher prevalence rate (SC and ST in India and black people around the world) should get tested and get genetic counseling before they get married. Two persons with sickle cell trait should not marry each other.
2- Educational Awareness: Increasing awareness about SCD and implications of being a carrier is crucial in high prevalence communities. Individuals with the sickle cell trait usually do not have symptoms of disease but can pass the genetic trait and disease to their children.
Sickle cell disease is a chronic and debilitating disease. The present treatments are not that good. They mostly help to reduce the symptoms. Possibility of cure with gene therapy is in the distant future but we are not there yet. The best course for now is prevention; know your genetic status and if you are a carrier, do not marry someone who is also a carrier. FULL STOPP.
Reference
1- Scientific American. Innovation in Sickle Cell Disease. October, 2024, p- 81
2- Chat Gpt
3- CDC.GOV/sickle cell disease
4- Sickle Cell Institute, VIMSAR, Burla https://www.vimsar.ac.in/departments/sickle-cell-clinic.php
About the Author
Dr Sahu is a pediatrician and 1969 graduate of AIIMS. He saw his first case of sickle cell disease in 1970 during his pediatric training in US.